In 2024 thanks to donors and fundraisers Secondary1st funded the first year of a research project led by Professor Simak Ali at Imperial College London investigating how changes in the ER gene contribute to hormone therapy resistance. About 44,000 people are diagnose with ER (oestrogen receptor) positive breast cancer each year in the UK and can be treated with hormone therapy but sometimes this treatment fails to work or stops working after a time, which can lead to the cancer spreading. Professor Ali and his team have now reported on their progress; understanding why some cancers resist hormone therapy will help to develop better treatments.
Research Background
Each year in the UK, around 44,000 people are diagnosed with oestrogen receptor (ER) positive breast cancer. These tumours have alterations in the ER gene which result in cancer cells using the hormone oestrogen to grow and survive. Many of these tumours can be successfully treated with hormone therapy which blocks the cells from using oestrogen, but around 40% of ER-positive tumours don’t respond to this treatment or stop responding over time. This can lead to the breast cancer coming back and spreading to other places in the body. This is secondary breast cancer, and it’s currently incurable. Scientists need to understand why some breast cancers are resistant to hormone therapy, so that they can find better treatments.
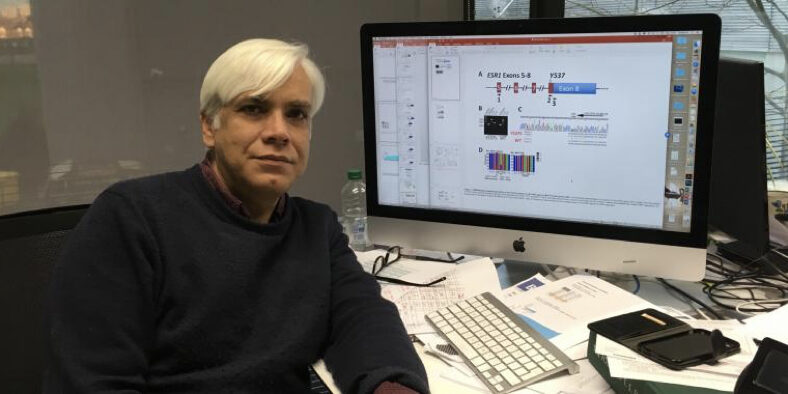
Professor Simak Ali and his team at Imperial College London are investigating how changes in the ER gene contribute to hormone therapy resistance.
Research Update
Changes in the ER gene can be found in many breast cancers which are resistant to hormone therapy. These changes mean the breast cancer cells no longer rely on oestrogen for their survival so hormone therapies are no longer effective in stopping their growth.
Professor Ali’s team have already developed state-of-the-art technologies to study the 10 most common ER gene changes in the lab. The team have found that the different changes in the ER gene affect breast tumour cells in diverse ways and they want to understand why.
So, to investigate this, the team are using breast cancer cell lines. Cell lines are used by scientists to grow cancer in a dish and research how they survive and respond to drugs. Multiple different cell lines are available based on which gene changes they have and the tumour they were originally sampled from. These differences can impact how the cell lines grow and survive. So, researching more than one cell line at a time allows scientists to show how general their findings are to breast cancer.
The team had previously engineered one breast cancer cell line to have these individual ER gene alterations. And in the last year they have made 9 out of 10 ER gene changes in an additional cell line. They are now creating the final ER gene altered cell line. If they find similar results in both of the cell lines, this will increase the confidence in their findings.
The team are now investigating how these two different cell lines grow when they have an ER gene change, and they will test how the lines respond to hormone therapy and other cancer treatments. This will help them understand how the different ER gene changes impact breast cancer cells and which drugs are most effective to stop their growth.
Finally, to investigate the ER gene changes in an additional way, the team have made a cell line which makes the altered ER gene only when the cells are treated with a certain drug. This will allow the researchers to control when the cancer cells are altered and understand what is different about the cells after this gene change. The team are now measuring the impact of the gene changes in the breast cancer cell lines growing in the lab.
What this Means for People with Breast Cancer
It is estimated that more than 61,000 people are currently living with secondary breast cancer in the UK. Many have oestrogen-positive breast cancer that has become resistant to hormone therapy. Understanding how altered ER genes contribute to hormone therapy resistance could lead to better treatments for people at risk of therapy resistance and those with secondary ER-positive breast cancer who have relapsed.